More than 100 thought-leaders in the healthcare industry from both the US and Canada shared information last month about how eHealth practices are improving patient care and what needs to be done.
Organized by the CTA Health IT accelerator (Consulate General of Canada), the Digital Healthcare Innovation Summit was co-hosted by Thomas Jefferson University where the discussions took place. Here, we outline some of the outcomes of the event.
Conclusions?
- Both the US and Canada are struggling with similar pressures including rising total health care costs as a percentage of GDP, and the challenge of interpreting the high volume of data generated by new health care technologies.
- eHealth technology is making an impact, especially in the areas of homecare, readmissions and medication adherence. But it needs to be well-designed, easy-to-use and solve patient treatment problems.
7 Conference Takeaways from Keynote Speakers and Panelists:

Keynote speakers Glen Geiger (left) Chief Medical Information Officer of Ottawa Hospital (left) and John C. Kairys (right) Chief Medical Information Officer of Jefferson University
1. The problem of data overload
- “Data volume is so great, no human being can manage it. We need a smart solution to handle it,” says Glen Geiger, Chief Medical Information Officer of Ottawa Hospital. “Primary care is going to be impacted by analytics.”
- “As my CIO, Praveen Chopra has observed, hospitals are typically rich in data but not rich on insights. Context is one of the big challenges for patient-collected data” says John. C. Kairys. “Data has to have meaning — it needs to be actionable at point of care. Extra data doesn’t help if it isn’t accurate.”
- “Physicians don’t want to be overwhelmed by data raining into the EMR,” says Dr Richard Snyder, SVP and SMO of Independence Blue Cross. “Frankly they are too busy to worry about a lot of new data.”
2. The need to “Get Modern”
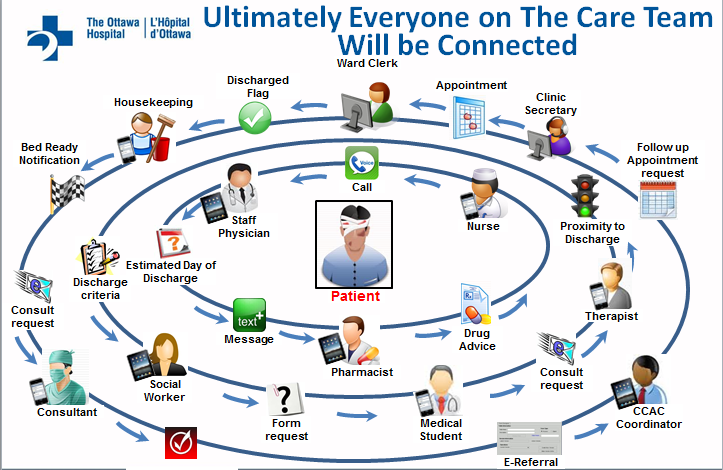
- “Surround the patient with fully integrated smart technology, for example use patient bar codes, smart beds,” says Glen Geiger. “The Industry can do better…there is a huge opportunity in healthcare today.”
- “Make the process fully electronic from end to end… from electronic orders, scheduling, imaging, surgery, to moving the patient,” says Glen Geiger. “Think in terms of how to streamline this action.”
- “Deloitte has estimated that within the next few years, one of every six patients will be seen virtually,” predicts John C. Kairys.
“Think in terms of how to streamline the process,” says Glen Geiger of Ottawa Hospital
3. The challenge of healthcare economics
- “The (cost) curve is rising relentlessly, and it can’t keep rising,” says Geiger. “For it to drop, efficiency and quality need to be more of a driver than ever before.”
- “In real business, exchange of services is self-regulated with supply and demand, but not healthcare,” says Geiger. “Hospitals and governments have to become more active.”
- “The drivers are the same in the US as in Canada, the industry does not self-regulate. The US is more complex, but Canada is more bureaucratic and less nimble.”
The Digital eHealth Panelists:
From left to right: Moderater Todd Wallach, Life Sciences Entrepreneur and Executive; Dr Harm Scherpbier, Chief Medical Officer of Main Line Health; Shafique Shamji, Executive Vice President and Chief Information Officer, Ottawa Hospital; Peter Preziosi, PhD, RN, CAE, Global Healthcare Strategist, Verizon Communications, Inc; Dr. Rich Snyder, SVP and CMO Senior Vice President and Chief Medical Officer, Independence Blue Cross
4. mHealth Apps: The need for ease of use
- “There’s a lot of evolution in the app market, but not everyone is going to stick to using them – 80% are abandoned in two weeks – people play with them and then they get tossed in a drawer.” says John C. Kairys. “We need devices that are easy to use and that promote on-going customer engagement.”
- “Developers need to explore and understand the EHR vendor's API. You have to take time to do that. Don’t simply bring us your device, but help us integrate it into our environment in a cost-effective and timely manner.”
- “There’s a tendency for developers to over-promise and under-price,” he points out. “If the product isn’t well thought-out and well-planned, there can be a lot of scope- and cost- creep.”
- “The cost of building interfaces is far greater in terms of dollars, time and human capital than vendors will ever tell you,” agrees Dr. Rich Snyder.
5. The need to improve workflow/ EMR etiquette
- “Medical records are full of duplicate entries, incorrect entries…who is going to curate this? Who is responsible for making sure data is accurate?” says John C. Kairys. “We need education and intelligent systems to present harmonized, coherent information.”
- “Most patient workflow has been designed organically, which means it’s terrible,” says Geiger. “It needs to be redesigned.
6. The importance of Philadelphia
- Says Dr. Femida Gwadry-Sridhar of Pulse Infoframe: “By being in Philadelphia we have access to global networks, there is so much opportunity here. We know that Philadelphia is also the starting point to the rest of the Washington-New York corridor.”
- Amos Adler, CEO of MemoText: “It’s a city that connects data, and it has a vibrant innovation scene. People are open to new ideas and are innovative here—but you have to have your A-game in place when you show up to succeed in Philadelphia.”
7. Future considerations
- “We have a fragmented health care system. We have an organizational problem first, and a technology problem second,” says Dr. Harm Scherpbier, Chief Medical Information Officer of Main Line Health.
- “Cybersecurity is becoming a greater concern in healthcare as health information becomes digitized and greater adoption of health technologies get integrated into the care process,” says Peter Preziosi, Global Healthcare Strategist for Verizon Communications.“Verizon’s 2014 Data Breach Investigative Report finds that 73% of all cybersecurity incidences in healthcare stem from 1) physical theft or loss of equipment, 2) insider and privilege misuse in accessing network data, and 3) sending information to the wrong places.”
The success of the Digital Healthcare Innovation Summit: An exchange of best practices and experiences
“This kind of exchange of ideas between the US and Canada is very helpful for healthcare practitioners here in the US and in Canada,” comments Donna Gentile O’Donnell, Vice President for Innovation Partnerships and Programs at Thomas Jefferson University about the event.
“Canada as a nation and a marketplace is an important neighbor and Jefferson is committed to the global marketplace of ideas and practice…we look forward to more events like this in the days ahead,” she says.
The most prominent commonality is the focus on the patient
“I found the Summit to be very informative and productive,” comments Shafique Shamji, the Executive Vice President and Chief Information Officer at Ottawa Hospital. “Because I have been fortunate enough to work in both the US and Canada, I was aware of some of the differences. However, it is truly amazing that at the end of the day, it’s the commonalities that matter most — the most prominent commonality is the focus on the patient.”
“Certainly there are different approaches and different drivers,” says Shamji. “However, the commonalities are what help create strong bonds between the health care providers in both countries.”
The Canadian Technology Accelerator Health IT for health information technology (CTA Health IT) in Philadelphia is operated by the Consulate General of Canada. The program helps connect innovative tech companies to international investments and market growth opportunities. For more information: www.ctaconnects.com @ctahealthIT. This article is reprinted with permission.
The nuviun blog is intended to contribute to discussion and stimulate debate on important issues in global digital health. The views are solely those of the author.


